Background
What are carbapenems? 
Carbapenems are a class of broad-spectrum antibiotics reserved to treat serious multidrug-resistant infections. Carbapenems are often considered antibiotics of last resort to treat an infection. This antibiotic class includes the following generic names: doripenem, ertapenem, imipenem, and meropenem.
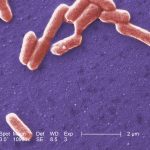
Which organisms can become carbapenem-resistant? 
All organisms have the potential to become resistant to carbapenems. Organisms of greatest concern include the Enterobacteriaceae family. Common organisms in this family include E. coli and Klebsiella species. Other organisms that can become resistant to carbapenems that are highly concerning include Acinetobacter and Pseudomonas species.
 Why should I be concerned about carbapenem-resistant organisms (CROs)?
Why should I be concerned about carbapenem-resistant organisms (CROs)?
Infections that are resistant to these antibiotics are very difficult to treat. CDC considers these types of antibiotic-resistant infections an urgent threat in the United States. CROs may cause a variety of infections, ranging from gastrointestinal illness and pneumonia to invasive infections of the bloodstream or organs.
What are the risk factors for getting an infection caused by a CRO? 
Healthy people usually do not get CRO infections. Patients who require devices like ventilators (breathing machines), urinary (bladder) catheters, or intravenous (vein) catheters; patients who are taking long courses of certain antibiotics, patients who are immunocompromised; and patients who have received international healthcare are most at risk for CRO infections.
 How are CRO infections transmitted?
How are CRO infections transmitted?
CRO is spread through contact with infected or colonized people, particularly contact with wounds, stool or contaminated hands or devices.
Infection Prevention
Decreasing antimicrobial resistant infections, such as carbapenem-resistant organisms (CROs) and carbapenemase-producing organisms (CPOs), require antimicrobial stewardship efforts and infection prevention measures. Intensity of infection prevention measures is based on mechanism of carbapenem resistance (CPO vs non-CPO), patient’s clinical status, and factors that increase risk of transmission to other patients in the facility. VDH recommends following the below guidance documents.
- Some CROs are caused by a specific resistance mechanism called carbapenemases, which are enzymes that directly break apart the carbapenem antibiotic making it ineffective.
- Because carbapenemase genes are often located on mobile genetic elements (e.g., plasmids), transfer of resistance among/across Enterobacteriaceae or other gram-negative organisms is enhanced, resulting in the potential for widespread transmission.
- Those organisms are called carbapenemase-producing or "CP."
- To slow the spread of CPOs, VDH recommends following the CDC Containment Strategy.
Infections caused by CPOs have been identified in all Virginia regions. Carbapenemase genes that have been identified in the United States are presented in Table 1. Determining the carbapenemase gene responsible for carbapenem resistance is critical to the public health response and for clinical decision-making.
Table 1. Carbapenemase Genes
|
Carbapenemase |
Comments |
|---|---|
| Imipenemase metallo-β-lactamase (IMP) | Endemic to areas outside of the United States |
| Klebsiella pneumoniae carbapenemase (KPC) | Most widespread in the United States; more commonly seen in Enterobacteriaceae compared to other gram-negative organisms |
| New Delhi metallo-β-lactamase (NDM) | Endemic to areas outside of the United States; increasing reports of United States residents without international healthcare exposure |
| Oxacillinase-type carbapenemases (OXA) | Different subtypes such as OXA-48 or OXA-23 |
| Verona Integron-encoded metallo-β-lactamase (VIM) | Endemic to areas outside of the United States; more commonly seen in Pseudomonas spp. that produce a carbapenemase |
In Virginia, a systematic public health response and investigation occurs upon identification of every CPO case. The public health response involves:
- Promptly detecting the presence of carbapenemases in clinical specimens or pan-resistant isolates;
- Collecting the least amount of information needed to determine appropriate recommendations based on CDC Containment Strategy Guidance;
- Verifying appropriate infection control measures (e.g., contact precautions, private room) are implemented by the healthcare facility to stop transmission, and performing onsite assessments of infection prevention practices;
- Identifying affected patients, determining whether transmission to other patients is occurring or has occurred, and recommending appropriate infection control measures to stop further transmission;
- Facilitating colonization screenings of high-risk healthcare contacts so that additional infection prevention measures can be put into place; and
- Continuing to work with the facility or setting on enhanced surveillance and implementation of infection prevention practices.
Reporting Requirements
Introduction
The State Board of Health updated the Virginia Regulations for Disease Reporting and Control (12 VAC 5-90-80) effective November 14, 2018. Carbapenemase-producing organisms (CPOs) were added to the reportable disease list and conditions reportable by directors of laboratories. Thus, the responsibility for reporting the presence of these organisms rests with physicians, directors of medical care facilities, and directors of laboratories. Because of the special laboratory testing needed to identify and confirm these organisms, however, it is expected that laboratories will be the primary responsible party for reporting these organisms. A further complexity exists because of the differing levels of capacity for identifying and/or confirming the presence of these organisms in laboratories. The guidance below is intended to clarify requirements for reporting and for submitting isolates for further public health testing.
Definition
Carbapenemase Producing Organisms (CPO) are defined as organisms where the isolate is:
- Positive for carbapenemase production by a phenotypic method (e.g., mCIM, Carba NP)
-OR- - Positive for a known carbapenemase resistance mechanism by a recognized test (e.g., PCR, X-pert CarbaR)
Reporting
Virginia Reportable Disease List in PDF Format
Report all carbapenemase-producing organisms (CPO), infection or colonization, to your local health department (LHD)
- Submit a laboratory report and/or Epi-1 form; see Table 1.
- Include available antimicrobial susceptibility testing (AST) results.
Submit carbapenem-resistant Enterobacteriaceae (CRE) and carbapenem-resistant Pseudomonas aeruginosa (CRPA) isolates to the Division of Consolidated Laboratory Services (DCLS) for further public health testing unless the laboratory is capable of conducting a comparable level of testing for carbapenemase-production as DCLS; see Table 1. This additional testing is not available for other CROs at this time.
- Use the DCLS Clinical Microbiology/Virology Request Form.
- Include available AST results with specimen submissions.
Table 1. Recommendations for Isolate Submission to DCLS and Reporting to LHD Based on Hospital/ Reference Laboratory Testing and Electronic Laboratory Reporting (ELR) Capacity
| Laboratory Testing and ELR Capacity | Isolate Submission and Reporting | ||
|---|---|---|---|
| CRE and CRPA testing capability | ELR capacity | Send CRE and CRPA isolate to DCLS? | Reporting Method to LHD for CPO^ |
| Unable to perform phenotypic/molecular testing comparable to that conducted by DCLS | Yes | Yes | Not applicable for CP-CRE and CP-CRPA; DCLS reports results to LHD. All other confirmed CPOs should be reported via ELR. |
| No | Yes | Not applicable for CP-CRE and CP-CRPA; DCLS reports results to LHD. All other confirmed CPOs should be reported via Epi-1 form and/or lab report. |
|
| Able to perform comparable phenotypic/molecular testing comparable to that conducted by DCLS+ | Yes | No* | ELR of carbapenemase-production result. |
| No | No* | Epi-1 form and/or lab report for carbapenemase-production result. | |
^ Hospitals using an out-of-state reference laboratory must include these findings in the ELR messages if their laboratory information system is able to do so. If not, submit to public health by fax or mail.
+ Please contact the HAI/AR Program to inquire if your laboratory can be exempt from sending CRE and CRPA isolates for further testing at DCLS.
* Per agreement with Virginia Department of Health, except when requested for further public health testing.
- Identify CRE and CRPA isolates that produce a carbapenemase and classify the type of carbapenemase present.
- Identify early, high-priority results that would require immediate notification to the Centers for Disease Control and Prevention (CDC), and be potentially characterized further at the regional antibiotic resistance laboratory or CDC:
- Pan-resistance
- CP-CRE with resistance mechanism other than Klebsiella pneumoniae carbapenemase (KPC)
- Any CP-CRPA
- mcr-type resistance
- Suspected novel resistance mechanism
- Facilitate submission of isolates with high-priority results to the regional antibiotic resistance laboratory or CDC for additional testing.
Testing algorithm conducted at DCLS for Enterobacteriaceae and P. aeruginosa isolates that meet carbapenem AST results requirements (refer to DCLS CRE/CRPA testing instructions)
- Confirm species identification by MALDI-TOF (Bruker Biotyper)
- Antimicrobial susceptibility testing (AST) by broth microdilution for all CRE and mCIM-positive CRPA
- Phenotypic testing for carbapenemase production by modified carbapenem inactivation method (mCIM)
4. Molecular detection of resistance mechanisms (KPC, NDM, OXA-48-like, VIM, IMP, mcr-1 and mcr-2) by real-time PCR for all CRE and mCIM-positive CRPA
Refer to DCLS CRE/CRPA testing instructions
- Submit pure suspect CRE or CRPA isolates on slant or plate media. Ship isolates at room temperature.
- Submit a completed DCLS Clinical Microbiology/Virology Request Form and AST results for each isolate. Testing will be delayed if AST results are not received.
- Turnaround time for reporting results will be within 6 business days of specimen receipt.
- Alert value results will be verbally reported within 1 working day of results. Non-alert-value, positive results will be verbally reported within 2 working days of results.
- A hard copy report of final test results will be provided to the submitter by mail.
Public Health Response
Upon confirmation of CP-CRE or CP-CRPA, the local health department will work with the facility/provider to implement the CDC Containment Strategy for Novel or Targeted Multidrug-resistant Organisms by:
- Identifying transmission is occurring;
- Identifying affected patients, such as roommates and high risk healthcare contacts;
- Ensuring appropriate control measures are promptly initiated/implemented to contain potential spread; and
- Characterizing the organism or resistance mechanism in order to guide additional response actions, patient management, and future responses.
For more information, please see the VDH HAI High Sign Special Edition on Carbapenemase-Producing Organisms
Contact the HAI/AR Program for questions or discussion.
Last Reviewed: November 2019. VDH will review this interpretive guidance annually at a minimum, and as needed due to regulation changes.
Impact in Virginia
Infections caused by carbapenemase-producing organisms (CPOs) have been identified in all Virginia regions.
Virginia CPO Case Counts
Click here for our quarterly CPO report.
National Testing Data
Emergency Department Care Coordination System
The Emergency Department Care Coordination (EDCC) Program was established in 2017 to provide a statewide technology solution that connects healthcare facilities, including acute care hospitals and post-acute care facilities. EDCC now includes MDRO flags for Candida auris and Carbapenemase-producing Organisms (CPOs), but facilities should still communicate MDRO status on transfer as the alerts are not real-time and only include information for Virginia patients and residents known to VDH. The flags are not intended to replace recommended communication, but to provide an additional layer of information.
Resources
Opens pdf to download
Opens document to download
Opens in a new window
External link will open in new window. Click link to exit Virginia Department of Health Website.
