State Health Commissioner Karen Shelton, MD, is newly appointed to her role leading the Virginia Department of Health, (VDH), but she isn’t new to public health or to Virginia. She’s a native Virginian who formerly was Director of the Mount Rogers Health District and Acting Director for Lenowisco and Cumberland Plateau Health Districts. She also served in the role of vice president and chief medical officer at Bristol Regional Medical Center before her appointment as state health commissioner.
Dr. Shelton holds a Bachelor of Science degree from Wake Forest University and a Doctor of Medicine degree from the University of Virginia. She completed her residency in obstetrics and gynecology at Eastern Virginia Medical School.
Having lived in several areas of the state and serving in several roles has helped shaped her perspective on the role public health plays for all Virginians, especially given modern challenges facing the Commonwealth such as the opioid crisis. Dr. Shelton is a mother of two grown daughters.
The VDH Office of Communications sat down with Dr. Shelton to talk about her priorities for goals for protecting and promoting the health of all Virginians.
What are your top priorities as you begin your new role as state health commissioner?
It was thrilling when I started as Health Commissioner to be able to sign the declaration of the end of public health emergency for COVID19 for our state. We have been working the last three years on COVID-19 and now that it is decreasing, it is good to be able to turn our attention to other things. We do need to focus on our public health workforce – we need to retain and recruit to enhance our workforce. We have been through a lot with COVID, and we need to make sure we address our own wellness.
The Opioid Crisis and Fentanyl
We want to refocus, certainly, on our opioid crisis efforts. We started seeing a large increase in overdose deaths in 2016 across the Commonwealth. We had started some efforts and began to make some headway to decrease those deaths from 2017 to 2018. By 2019, we were beginning to see a decrease in those deaths. Unfortunately, they have skyrocketed again over the three years of COVID-19.
Substance use disorder increased, unfortunately, during COVID-19 and we’ve seen an increase in our overdose deaths. So, as we refocus our efforts on the opioid crisis, the governor has enacted his Executive Order 26, to crush the fentanyl crisis. We at VDH look forward to partnering with other agencies across the state as we tackle this problem. We want to focus on education, prevention, harm reduction, treatment and anything that we can do to combat overdoses as well as substance use disorder.
In doing so, we are always asking how we can reach those with substance use disorder, how we can help them and how can we guide them toward recovery when they’re ready. And then what are the recovery options that we have for them and how do we reduce the harm during their time of need until they are ready to get to recovery?
Also, we look at the people who have been experimenting with drugs and who may overdose on a first-time use or infrequent use of drugs. How do we combat that as well? We have a lot of initiatives ramped up and we also rely on education and prevention.
Naloxone distribution is a huge effort across the state, so we’ll be working on that along with the many different efforts to combat the opioid overdose and addiction crisis that we have.
Maternal and Infant Health
As an OB/GYN, another main goal of mine is looking at maternal and child health issues. We want to have healthy families, moms and babies. As we focus on those efforts, we want to address issues of maternal and infant mortality. Specifically in maternal health, we want to address mental health, substance use disorder, chronic disease, intimate partner violence, and healthcare access. We are using data to inform our initiatives, and we have some great programs in our agency and partnerships with other agencies and community resources that are already addressing these issues, but we want to double down on our efforts and see if there are additional programs or initiatives that we can use to fill some gaps. I’m looking forward to championing these initiatives with our partners, along with the great work that is already going on within our agency.
The Public Health Workforce
Before COVID-19, a lot of people didn’t really know much about what we did as a public health workforce and all the wonderful programs that we have throughout the Commonwealth.
During COVID-19, we’ve had a trial of our public health workforce. We have people who are still with VDH who have worked tirelessly over the last three years to address COVID-19 for our state. We have a lot of people who came to work for our agency over that time and then a lot of people who have now left public health. We want to champion the public health workforce that we have and see what we can do to bring healing and resilience and to boost the energy again of those who are still working in public health. I look forward to getting out to visit the local health districts and connecting with them on what their needs are. We also are thinking about how we can recruit new people into public health., and looking at how we can get people excited about public health, how we get them into our workforce and champion with us for the best, the healthiest state in the nation.
How can citizens learn more about fentanyl and what can they do to help or to get involved?
Our local health departments have free naloxone and provide training on how to recognize an overdose, administer naloxone, and save a life. There are also REVIVE trainings that are offered in communities that are also a good way for people to learn about opioids, about addiction, and about how to recognize an opioid overdose., and how to save a life with naloxone.
Naloxone is a medicine that can temporarily reverse the effects of opioids. Opioids are very dangerous because when people take too much of an opioid, they stop breathing. And so that’s how they die. The naloxone blocks those receptors and allows people to start breathing again.
The REVIVE! trainings have been going on across the state for some time and I know the efforts will continue. As we get further into our campaign against overdose and addiction, that will be spreading more in communities.
How have all your roles – from doctor to health director to chief medical officer – shaped your perspective for this new role?
I feel like my new role is really to evaluate the health of the Commonwealth. Part of what I enjoy, being chief health strategist, is asking how do I make sure that the important services are covered not only for healthcare, but for the well-being of the community?
What is the access? How do we connect people to care? How do we get people to value their health?
I think that my time at the hospital really helped me understand a lot about what hospitals do to provide for our communities and how VDH partners with them. Not the least of those is our Community Health Assessments which are integral in our community when it comes to the overall health strategy of a community.
Also, while I was there (on the hospital side), I learned a lot working on the hospital side about quality initiatives. I learned a lot about patient safety initiatives, best practices, peer review, peer guidance. Part of that was asking how we make sure that our healthcare providers are performing at their best and learning how to guide them in their efforts.
In 2021, as I was leaving the Virginia Department of Health, we had rolled out the vaccines. We were working on outreach in areas that had not had the opportunity to receive the COVID-19 vaccines and we were making good progress. When I arrived at the hospital, Delta began to surge. We saw the highest numbers of cases that they had to that date at the hospital, followed by Omicron in the winter.
It’s important that we are refocusing now. I think as a Commonwealth it’s important to make sure people are getting back to taking care of themselves with routine primary care visits and preventive visits such as screenings for cancer and other diseases to make sure we’re taking good care of our health.
Continuing on that theme, how can Virginians continue to stay healthy now that we’re going to be living with COVID-19?
Well, COVID-19 is now a part of our community. It is worse than the flu. When we look at the outcomes, as far as the percentage of hospitalizations and deaths that have occurred from COVID-19 in comparison to the flu, it is an illness of significance for our communities. At the same time, so much of our population has been vaccinated. We do have a lot of immunity that, for most people, it’s not an extreme health concern. Certainly, for people who have certain medical conditions and those who are immunocompromised, that it is a significant factor.
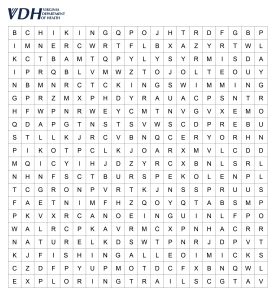
We all need to be aware, but most of us are now getting back to normal. I don’t know that it’s the same normal. But it’s important for people to get back to getting those mammograms, colonoscopies, and other screenings that healthcare providers recommend for their general health. One thing Virginians can focus on regarding their health is getting out and about. By that, I mean physical exercise, getting out and walking or doing the things you love. Get those breaths of fresh air and taking care of yourself that way.
Mental Health Focus
There has also been a lot more attention on mental health in our communities because of COVID-19. People experienced isolation and seclusion. They were not able to get out and about and to socialize. Now we have mental health repercussions. Fortunately, the stigma has been reduced in discussing mental health. I think people are a little bit more open now to talking about it. They want to know about the resources where they can seek help.
The state of Virginia and the Governor’s plan has looked at increasing our capacity for mental health services. And we do have the 988 line that people can call. This is a national number, but the state of Virginia is up and going with that faster than even the national plan.
So, we’re thrilled to have that resource in Virginia, and we know that health care providers do have resources for referral. I know that in the behavioral health world, they’re working a lot with “Right Help, Right Now.” They are focusing on educating people on where they can go in a crisis and how they can get the care they need at the time they need it.
We want people to focus on their own wellness, not only mental health, but also social wellbeing. As we look at our communities, part of public health is looking at social determinants of health. We look at whether people have a place to live, whether they have access to nutritious food, how they are educated and if they can make a livable income. We look at these things to see how, as public health workers, we can work with our resources and link people in our communities with those resources.
To learn more about the REVIVE! Opioid Overdose and Naloxone Education (OONE) program, visit the Department of Behavioral Health and Developmental Services website.
To contact your local health district or department and learn more about naloxone and REVIVE! Training, visit the VDH website.