National Black HIV/AIDS Awareness Day: February 7
National Black HIV/AIDS Awareness Day (NBHAAD) is observed on February 7 each year. It exists to raise awareness about the impact of HIV on Black and African American communities. It was first observed in 1999 and highlights the importance of decreasing stigma and increasing community involvement. Improving access to HIV education, prevention, testing, and HIV care are focuses of NBHAAD, as well.
Virginia data
As is the case across the U.S., Black and African American communities are more impacted by HIV in Virginia. In 2024, while Black/African American communities made up 19.12% of Virginia’s population, they accounted for 50.2% of new HIV diagnoses and 56% of people with HIV in Virginia that year. The figure below shows the rate of new HIV diagnoses by race and ethnicity per 100,000 persons. Using rates allows for the comparison across different population sizes.

You can find additional HIV, STD, and viral hepatitis data on our website.
Causes
According to KFF, several challenges may contribute to the epidemic among Black people. These include experiences with:
-
- Higher rates of poverty
- Lack of access to health care
- Higher rates of some sexually transmitted infections
- Lower awareness of HIV status
- Stigma and discrimination
- Combating Stigma
How can you help combat stigma? Talk openly about HIV to help normalize the subject. This helps others learn about HIV and correct myths and misinformation. The Centers for Disease Control and Prevention (CDC) has a stigma language guide that can help with these talks.
We can all help end HIV stigma through our words and actions in everyday life. Be a role model for positive and supportive behavior. Check out some scenarios from CDC to see how you can model positive behavior when you witness HIV stigma.
Access testing and prevention services near you
Free or low-cost HIV, STD, and viral hepatitis testing is available throughout Virginia. VDH funds local health departments, clinics, and community organizations to offer testing services if you do not have a primary care provider. To learn more about testing in Virginia or to find testing near you, visit our testing webpage.
PrEP (pre-exposure prophylaxis) for HIV is available as a pill taken daily, or a shot taken every other month or every six months. PrEP prevents getting HIV through sexual contact about 99% of the time when taken as prescribed. VDH provides funds to locations throughout the Commonwealth to offer HIV PrEP.
Additionally, there are also post-exposure prophylaxis (PEP) options to prevent HIV and STDs. PEP for HIV involves taking a course of medications to prevent HIV infection. It is critical that these medications are started within 72 hours of a potential exposure. DoxyPEP involves taking the antibiotic doxycycline after unprotected sex to prevent getting a bacterial STD. DoxyPEP is available at most local health departments.
If you’re interested in PrEP or PEP, visit our PrEP and PEP webpage to learn more or find a PrEP clinic near you. As noted above, nPEP is extremely time-sensitive, so please call your provider or our hotline if you believe you have been exposed to HIV and need PEP. To learn more about DoxyPEP, read our DoxyPEP fact sheet.
VDH’s response
VDH’s Division of Disease Prevention has multiple programs that address HIV prevention and treatment. This includes:
-
- Funding, oversight, resources, or support to local health departments, community, and/or clinical organizations for:
- HIV, STD, and viral hepatitis testing programs
- Patient linkages and referrals
- Education and outreach programs
- Comprehensive harm reduction programs
- Condom distribution
- PrEP, PEP, and DoxyPEP distribution
- Disease intervention services
- Data collection and follow-up
- Community planning groups
- HIV care services
- And more!
Learn more about the services that VDH provides on our website. If you want to become involved in any of our community groups, visit our Get Involved page.
Reach out for support
If you have any questions or need additional support, contact the Virginia Disease Prevention Hotline. Hotline counselors are available weekdays from 8 a.m. to 5 p.m. It is closed on Virginia state holidays.
The hotline number is (800) 533-4148 and is toll free.
Hotline staff can help connect you to programs and needed resources throughout Virginia.


 The Centers for Disease Control and Prevention (CDC) has announced another 12-month extension to the Strengthening STD Prevention and Control for Health Departments (STD PCHD) grant. The extension will cover the period of March 1, 2026, through February 28, 2027.
The Centers for Disease Control and Prevention (CDC) has announced another 12-month extension to the Strengthening STD Prevention and Control for Health Departments (STD PCHD) grant. The extension will cover the period of March 1, 2026, through February 28, 2027.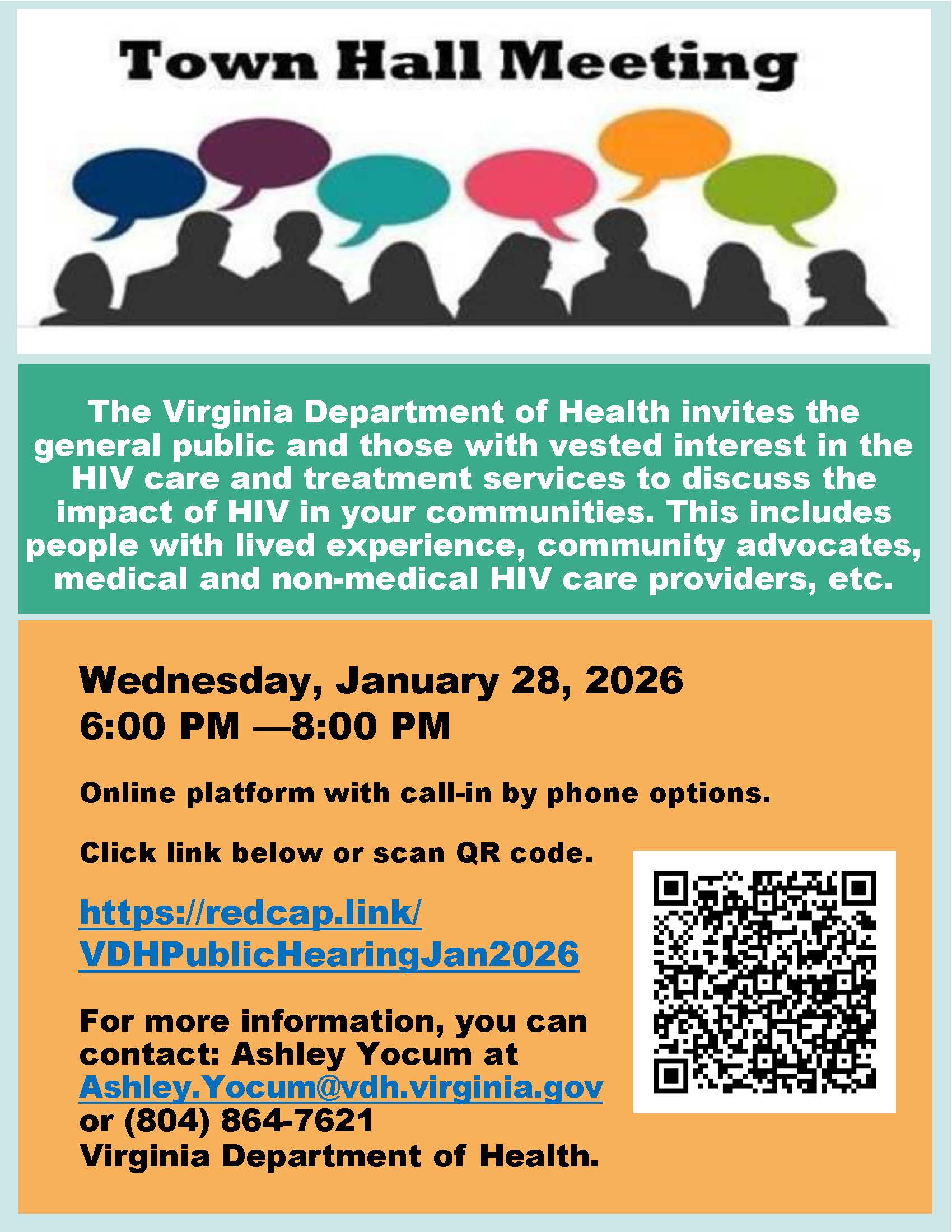







 What’s happening in Virginia?
What’s happening in Virginia?
 Mpox cases continue to occur primarily in men. Mpox also disproportionately affects communities of color. Mpox cases have occurred in all five state health regions, with the greatest number of cases reported from Virginia’s Northern and Central health planning regions (82%).
Mpox cases continue to occur primarily in men. Mpox also disproportionately affects communities of color. Mpox cases have occurred in all five state health regions, with the greatest number of cases reported from Virginia’s Northern and Central health planning regions (82%).

 On September 30, 2025, DDP received a surprising notice of award (NoA) for the HIV Medical Monitoring Project (MMP). Prior funding for MMP ended on May 31, 2025, and we were told the grant would not be renewed. Therefore, DDP ended the program and MMP staff were unfortunately laid off. Due to the unexpected nature of this new award, the back date of the project period to 6/1/25, and current federal government shut down, the remainder of the first year, or grant year 1, will be used to recruit staff and re-establish the program. DDP is awaiting further guidance from CDC, which will occur after the resolution of the federal government shutdown.
On September 30, 2025, DDP received a surprising notice of award (NoA) for the HIV Medical Monitoring Project (MMP). Prior funding for MMP ended on May 31, 2025, and we were told the grant would not be renewed. Therefore, DDP ended the program and MMP staff were unfortunately laid off. Due to the unexpected nature of this new award, the back date of the project period to 6/1/25, and current federal government shut down, the remainder of the first year, or grant year 1, will be used to recruit staff and re-establish the program. DDP is awaiting further guidance from CDC, which will occur after the resolution of the federal government shutdown. DIS (Disease Intervention Specialist) Recognition Day was Friday, October 3. This special day is observed nationally each year to promote the special work that our DIS do within our communities. The National Coalition for STD Directors, VDH, and DDP had blog postings for the occasion and promoted or shared posts and graphics on social media.
DIS (Disease Intervention Specialist) Recognition Day was Friday, October 3. This special day is observed nationally each year to promote the special work that our DIS do within our communities. The National Coalition for STD Directors, VDH, and DDP had blog postings for the occasion and promoted or shared posts and graphics on social media. The Resource Connections website is being relaunched with a fresh new look and a new name — The RC: Resource Connections — on the Connect 211 platform! Along with the updated design, the site will feature a new logo and URL.
The Resource Connections website is being relaunched with a fresh new look and a new name — The RC: Resource Connections — on the Connect 211 platform! Along with the updated design, the site will feature a new logo and URL.
 DIS are trained public health professionals with varied backgrounds and skill sets. They’re a group of public health specialists who identify, locate, and prevent the transmission of infections. They often have experience in community health, social work, health education, outreach, public health, and lived experiences.
DIS are trained public health professionals with varied backgrounds and skill sets. They’re a group of public health specialists who identify, locate, and prevent the transmission of infections. They often have experience in community health, social work, health education, outreach, public health, and lived experiences.
 The Virginia Community HIV Planning Group (CHPG) needs new members. The CHPG works with DDP to develop and monitor Virginia’s Integrated HIV Services Plan. Their main goal is to end the HIV epidemic and improve the health of people with HIV. The Plan will guide DDP work over the next five years.
The Virginia Community HIV Planning Group (CHPG) needs new members. The CHPG works with DDP to develop and monitor Virginia’s Integrated HIV Services Plan. Their main goal is to end the HIV epidemic and improve the health of people with HIV. The Plan will guide DDP work over the next five years. Bulk condom orders are currently on hold while the Department of General Services negotiates with Global Protection to renew its contract with the Commonwealth of Virginia. This situation has extended beyond initial expectations, resulting in temporary shortages of several brands, including non-latex condom options, lubricant, and Trojan Magnum condoms.
Bulk condom orders are currently on hold while the Department of General Services negotiates with Global Protection to renew its contract with the Commonwealth of Virginia. This situation has extended beyond initial expectations, resulting in temporary shortages of several brands, including non-latex condom options, lubricant, and Trojan Magnum condoms.