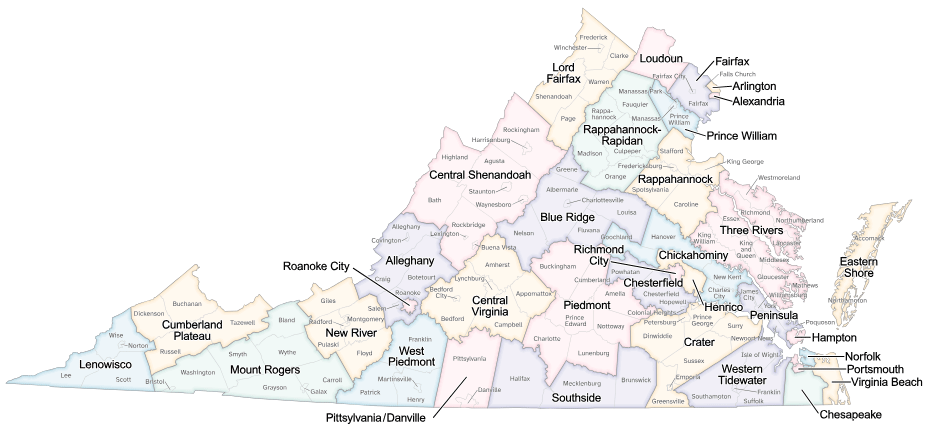
- Alexandria
- Alleghany
- Arlington
- Blue Ridge
- Central Shenandoah
- Central Virginia
- Chesapeake
- Chesterfield
- Chickahominy
- Crater
- Cumberland Plateau
- Eastern Shore
- Fairfax
- Hampton
- Henrico
- Lenowisco
- Lord Fairfax
- Loudoun
- Mount Rogers
- New River
- Norfolk
- Peninsula
- Piedmont
- Pittsylvania/Danville
- Portsmouth
- Prince William
- Rappahannock
- Rappahannock/Rapidan
- Richmond
- Roanoke
- Southside
- Three Rivers
- Virginia Beach
- West Piedmont
- Western Tidewater
Last Updated: October 14, 2025